Before we start talking about thyroid hormone it is important that we first define what a hormone is. Hormones are chemical messengers. They travel through the bloodstream to their target tissue and once there they bind to a special receptor on a cell. This binding effectively delivers the message. As a result of this, changes happen within the cell to carry out the commands that were relayed by the message. We have hundreds of hormones in our bodies helping us function and respond to our environment.
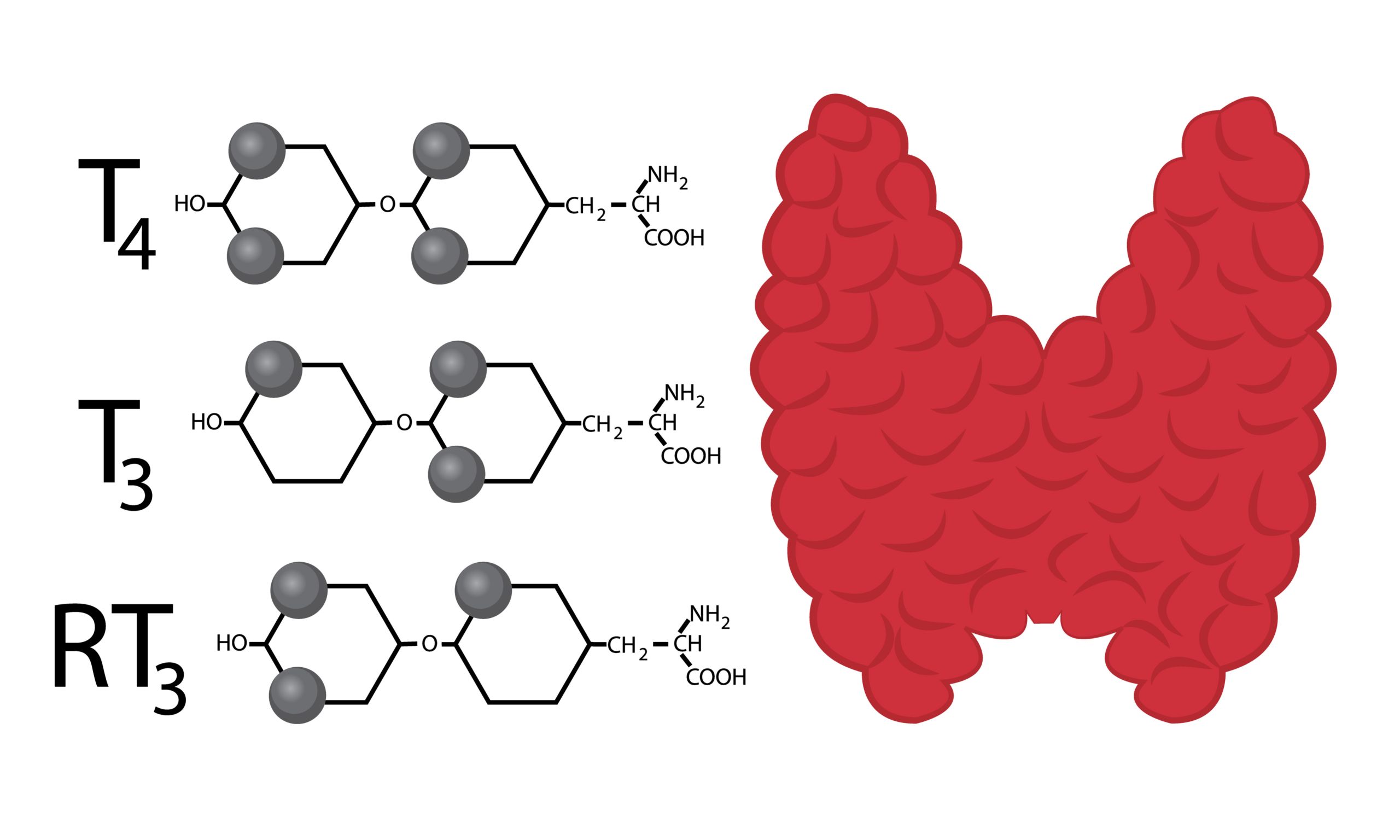
An important hormone I am often asked about is thyroid hormone. There are 2 main types of thyroid hormones in the body named T4 and T3 (in case you were wondering the number indicates the number of iodine atoms attached to the hormone structure). These are made by the thyroid gland which sits at the base of the neck. The main function of T4 and T3 is to regulate our metabolism. Every organ in our body contains thyroid hormone receptors. As such, thyroid hormone levels affect not only the rate at which we burn calories, but also many other things including heart rate, body temperature, brain function, hair and skin, muscle function, movement of the GI tract, and the function of other hormones.
The most common thyroid problem, and the primary focus of this article, is hypothyroidism. Hypothyroidism can cause a host of symptoms including fatigue, weight gain, slow heart rate, elevated cholesterol levels, cold body temperature, impaired memory/cognition, muscle weakness, muscle stiffness, joint aches, depression, hair loss, dry skin, irregular menstrual periods and fertility issues in women and constipation. These symptoms often develop slowly over time.
It is estimated that 4.6% of the population over the age of 12 has hypothyroidism. Hypothyroidism is more common in women (1 in 8 women will develop hypothyroidism during their lifetime) and it gets more prevalent as we get older. I would argue that hypothyroidism is even more prevalent than this suggests. One reason is that the “normal” reference range for thyroid labs provided by the lab companies are far from optimal ranges for most of us. For example, most labs list a normal range for TSH from 0.4-4.5 mIU/L where optimally, this range is from 0.3-2 mIU/L.
A second reason it that it is very unusual to have a complete thyroid lab panel performed. Typically, your “thyroid level” is measured by checking a TSH (thyroid-stimulating hormone) level, and if you are lucky, a free T4 test. But, there is much more to the picture. I recommend everyone get a panel that includes TSH, free T4, free T3, reverse T3, and thyroid antibodies. Depending on the results, further testing may then be needed.

Given thyroid hormone levels play such an important role in our overall health it is important that our thyroid levels are optimized. To better understand these tests, we need a little knowledge of the regulation and flow of thyroid hormones. The amount of thyroid hormone in the body is under the control of the pituitary gland which is in the brain. The pituitary gland monitors the levels of T4 and T3 in the bloodstream and in response, alters the amount of TSH (thyroid-stimulating hormone) it releases. As the name implies, TSH is the hormone that tells the thyroid gland to make more T4 and T3. If the pituitary senses that thyroid hormone levels are low, it increases its production of TSH which stimulates the thyroid gland to make more T4 and T3 and vice versa.
In response to TSH, the thyroid gland makes and releases mostly T4 (about 90% of what it makes) and a small amount of T3 (about 10% of what it makes). T4 and T3 carry the same message to the cells but T3 is about 7 times more powerful than T4. Because of this, the body controls T3 levels more tightly by more rapidly breaking down T3 in the bloodstream. As T4 reaches its target organs there is an enzyme that pulls off an iodine changing it to T3 so T3 can exert its more powerful effect on the cell. Most T4 and T3 are carried through the bloodstream attached to a protein named thyroid-binding globulin. The thyroid hormone attached to this is not available to bind to thyroid receptors in the cells. What we are most interested in is the amount of free hormone available to bind to receptors.
T4 can also be changed into reverse T3 (rT3) which is a mirror image of T3. rT3 will bind to the T3 hormone receptor on cells, however, instead of turning on the cell as T3 does, it just sits there and blocks the site.
The most common cause of hypothyroidism in the United States is actually an autoimmune disease named Hashimoto’s thyroiditis. In this condition, the body’s immune system attacks the thyroid gland tissue leading to increased thyroid damage over time. Thyroid antibody tests evaluate for this particular condition. Often, patients with hypothyroidism do not even know if they have autoimmune thyroid disease and if they do know this then they are generally told just to take thyroid hormone. However, If this is present, it is important that the autoimmune condition itself is addressed. We can do things to stop this process and halt further thyroid damage. Another important reason to address this is to prevent the development of other autoimmune diseases, It is well known that the presence of one autoimmune condition puts a patient at an increased risk of developing other autoimmune conditions
Other causes of hypothyroidism:
- Decreased nutrients needed to create thyroid hormone. To make T4 and T3 we need adequate levels of various nutrients including tyrosine, iodine, iron, zinc, selenium, vitamin D, Vitamin C, and B vitamins. Our diets are not as nutrient-dense as they used to be so it is possible that we do not have enough intake of some of these. The use of sea salt has led to decreased iodine in our diets and iodine deficiency is something that we are seeing more frequently. We can measure levels of these nutrients in the body if a patient is hypothyroid.
- Toxins that block the production of thyroid hormone. Our environment is full of endocrine-disrupting chemicals that interfere with hormone synthesis. These include plasticizers, pesticides, and heavy metals. If these are present, it is important to minimize ongoing exposure and to properly detox.
- Stress. Stress itself can impede proper thyroid hormone production.
- Genetics. Some of us have genetic changes decreasing our ability to make the deiodinase enzyme that converts T4 to T3. This results in a decreased amount of T3, the most powerful thyroid hormone, and is often not reflected by the TSH. For these patients, it may be necessary to replace T3 and not just T4 which is what is generally prescribed.
- An elevated rT3. As mentioned above if there is an imbalance between the amount of T3 and reverse T3 the T3 binding sites will be blocked making the cell essentially hypothyroid. This imbalance can be seen in trauma, infection, inflammation, stress, and severe calorie restriction.
Many of us are unaware of the important role that the thyroid plays throughout the entire body. If your goal is to optimize your health, then finding your proper thyroid balance is essential. I would recommend you work with a functional medicine provider to obtain a full picture of your thyroid health. The full thyroid panel will likely not be covered by insurance but can be obtained for a very reasonable price through self-pay labs.
This article is meant to inform readers of the importance of thyroid function and about lab testing that is available. It is not meant to constitute personal medical advice. Always consult your medical provider regarding labs, treatments, and supplements.